 Before I was 10 days old I may well have earned a nickname: “Fountain Fred”. Or, because I was actually born in the Netherlands, “Free de fontein“. I had a stomach blockage, infant pyloric stenosis (“PS”), almost from birth. This meant spectacular projectile vomits of all my mother’s milk, quickly increasing in frequency and power.
Before I was 10 days old I may well have earned a nickname: “Fountain Fred”. Or, because I was actually born in the Netherlands, “Free de fontein“. I had a stomach blockage, infant pyloric stenosis (“PS”), almost from birth. This meant spectacular projectile vomits of all my mother’s milk, quickly increasing in frequency and power.
 Not just the “wet burps”, “baby puking” or “a bit of reflux” that all babies have. Not just a cute spit like the top picture shows, but fire-hose stuff, reaching the wall, soaking unwary parents, and perhaps a sceptical and unsuspecting doctor who has been trying to assure the anxious parents that “all babies vomit”. A big and spectacular surprise for any casual bystander, but totally traumatic for my first-time parents.
Not just the “wet burps”, “baby puking” or “a bit of reflux” that all babies have. Not just a cute spit like the top picture shows, but fire-hose stuff, reaching the wall, soaking unwary parents, and perhaps a sceptical and unsuspecting doctor who has been trying to assure the anxious parents that “all babies vomit”. A big and spectacular surprise for any casual bystander, but totally traumatic for my first-time parents.
This blogsite is about a weird condition that causes several tiny bubs in every 1,000 to vomit violently and uncontrollably, how this condition and infant surgery have affected me and others, and how PS in babies can be recognized more promptly and treated better than they and their parents all-too-often are.
If you’ve experienced any of this, please consider sharing your story too –
* below my story here or
* on the “About” page, or
* under one of this Blog’s posts, or
* on one of Facebook’s busy PS Group pages.
Any comment or contact is most welcome: it may well be therapeutic for the reader with a PS history, and will certainly add to the wider and better awareness of this horrible, all-too-common but hardly known and often poorly diagnosed condition.
 On this “page” I give an overview of what PS looks like and how it’s usually treated, as well as something of my story. Sometimes you can click on an image if it’s too small for you to get its message. Many of these images are taken from the web and in the public domain as far as I have been able to check. Although I’m a blogger not receiving any income from my interest, do let me know if (further) acknowledgement or withdrawal of an image is deemed necessary.
On this “page” I give an overview of what PS looks like and how it’s usually treated, as well as something of my story. Sometimes you can click on an image if it’s too small for you to get its message. Many of these images are taken from the web and in the public domain as far as I have been able to check. Although I’m a blogger not receiving any income from my interest, do let me know if (further) acknowledgement or withdrawal of an image is deemed necessary.
This is what pyloric stenosis looks like (the image is from a medical video on YouTube) . . . and I’m told this is a mild vomit. My late parents could never bring themselves to talk about their memories of my sickness… is that any wonder?
Ewww… yuck, Fred!
PS is popularly dubbed “projectile vomitting”: it is so forceful that milk shoots out, often in an arc and for 1, 2, or even 3 metres (and some report, “even 30 feet” (though that’s a bit hard to believe, it’s almost 10 m) and “even to the ceiling”! Whatever, we get the message, and it’s small wonder this unusual condition affects the parents so powerfully that they instinctively know: This is not normal “baby sick”.
In 1945, even grainy black-and-white photos were hardly affordable to my War-weary parents… and in those times people didn’t talk about life’s ugly things, let alone capture them on camera, so this web image of an unusually hapless Py baby keeps reminding me that PS is a truly scary condition that can end a baby’s life within days.

I was born in a small rural “city” (with just a few thousand inhabitants but city status) in the northern Dutch province of Friesland. As happened there in the 1940s, my proud father (as one of the place’s clergy) paid somebody to announce my birth to all the town notables… my parents were clearly very proud and pleased.
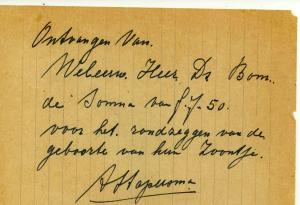
The City Messenger’s receipt (7.50 Dutch florins) for announcing my birth to the town’s leading citizens
Telephones were not yet everywhere, so my Dad sent cryptic telegrams to announce the long-awaited arrival to my grandparents who lived in faraway Amsterdam and Zeeland – at least “faraway” in 1945 shattered post-War Holland.
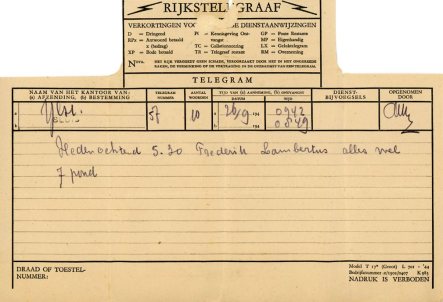
Sent from Ylst to Sluis. Translation: This morning 5:30 Frederik Lambertus all well 7 pounds
It is hard to imagine how utterly devastated my parents will have felt when the violence that is PS started just a few days later. Soon it was clear that their long-awaited little treasure was vomiting himself to exhaustion and death when less than a week old. The forcefulness of PS puking can sometimes cause bleeding in the stomach, create a hernia in the wall of the abdomen, and also damage the young and fast-developing brain.
This set of photos was not me either, but tells me that whenever my stomach performed like this it would have caused some consternation and apprehension. These waves of peristalsis are another clear sign of PS: you can see the stomach muscles trying to push food through the overgrown and blocked pyloric valve at the end of the stomach.
“Pylorus” is Greek for “gate”, and in PS the stomach’s exit gate ring-muscle (A) becomes thickened or hypertrophied (B), thus narrowing (‘stenosing”) and then often blocking the stomach’s exit passage. The full medical name of the condition is “infantile hypertrophic pyloric stenosis”… quite a mouthful that’s usually coded as IHPS, HPS, PS, or just Py. The cause is still only partially understood, and so there are several theories, most of them beyond my ability to understand. It’s possible there are in fact several possible causes – “a perfect storm”.
 One theory has been long studied and repeatedly argued: it’s one that is easier to understand and fits not only many of the medical observations of PS but also its characteristic and obvious symptoms and behaviour.
One theory has been long studied and repeatedly argued: it’s one that is easier to understand and fits not only many of the medical observations of PS but also its characteristic and obvious symptoms and behaviour.
This theory states that a higher level of acid in the gastric passage, combined with an anxious mother over-feeding her sick child, over-stimulates the pyloric ring muscle. This theory has been carefully explained in articles and since 2014 in 3 small books by the retired Scottish Prof. Ian M Rogers. His research has supported his theory that the prime cause of PS is an unusually high level of the hormone gastrin which stimulates gastric acid release into the stomach.
 In 2019 Dr Ian Rogers published an enlarged and updated book of almost 200 pages, Pyloric Stenosis of Infancy: the great Mystery Unravels, available from Amazon Books UK (not obtainable from other Amazon national branches). One of the additions is an overview of the history of the recognition and treatment of infant pyloric stenosis, and the book has an extensive bibliography.
In 2019 Dr Ian Rogers published an enlarged and updated book of almost 200 pages, Pyloric Stenosis of Infancy: the great Mystery Unravels, available from Amazon Books UK (not obtainable from other Amazon national branches). One of the additions is an overview of the history of the recognition and treatment of infant pyloric stenosis, and the book has an extensive bibliography.
The list of possible culprits that increase gastrin release is lengthy. Several genes are involved in about 20% of PS cases, but other common subversives have been shown to include erithromycin (a frequently prescribed antibiotic), maternal stress and anxiety, milk chemistry, Caucasian race, over-feeding, formula feeding, prematurity, mother’s age and smoking, baby’s sleep position, and other factors.
Recent reports implicate bottle feeding as a risk factor, and a formula’s chemistry is of course different from breast milk. Some earlier reports have claimed that bottle feeding reduces the risk of PS, perhaps because it makes quantity easier to control. Some statistics say older mothers are at greater risk of having a PS baby, others claim to have found a youthful first birth is more at risk, and yet others say maternal age is not a factor. Some reports have prematurity as a risk factor and others not. In other words, some risk factors seem to be clearly established and others are still debated, even after several hundred years of PS being recognized.
Again, not me! I am thankful that most PS babies don’t get to this awful degree of weight loss, hunger and dehydration. Just look at those arms and the neck. How I wish my Mum and Dad had taken some more photos, journalled, or just talked about what happened to me back in 1945. But I can understand: my country of birth had just been bled into poverty by the War and my parents would have avoided creating a photo record of this awful time.
The distressing web image below also shows the dangerous malnutrition (hunger) and
dehydration which PS sometimes causes before it is diagnosed and managed.
 Sunken fontanelles or the bones making up the baby’s skull (see right) are seen more commonly and are also a real danger sign. This early starvation can cause lifelong damage, especially to some of the brain’s functions. A recently published Australian study of 43 infants with IHPS found that at ages 1 and 3 years they scored significantly lower on four of the five Bayley subsets (cognitive, receptive and expressive language and fine motor) compared to control infants.
Sunken fontanelles or the bones making up the baby’s skull (see right) are seen more commonly and are also a real danger sign. This early starvation can cause lifelong damage, especially to some of the brain’s functions. A recently published Australian study of 43 infants with IHPS found that at ages 1 and 3 years they scored significantly lower on four of the five Bayley subsets (cognitive, receptive and expressive language and fine motor) compared to control infants.
Several earlier studies have reported similar findings, and I cannot but link them with the observation that several of my skills in these areas are clearly below those of my parents and four siblings. Despite this, I have lived well for 75+ years: “Fountain Fred” has been a survivor!
Poor diagnostic work is a concern not unrelated to starvation and brain damage. Countless parents have posted to several large social media sites or blogged about how very angry, frustrated and upset they were when doctors (often not just one) stalled in deciding on what had become obvious to them, especially when they themselves had had PS, if it was in the family, and/or after they had done their research homework and recognised many or all of the many well-publicised symptoms.
Doctors used to go by the usually clear physical signs of PS and (if known) the family history. Only sometimes was an x-ray called for to establish a suspected diagnosis beyond doubt. Now (again, judging by countless reports) too many doctors delay, belittle parents as jittery or inexperienced new parents, talk endlesslyabout “alternative diagnoses” and wait until costly imaging technology can be brought into play (ultrasound and xray tests etc) – all in the name of “the scientific approach”. One may suspect that the cashflow of the medical industry and the bogey of litigation for premature diagnosis may also play a part?
 Judging by the many reports online, PS babies all-too-often get to a very distressing and extreme condition before their PS is diagnosed. There may well be some “unspoken history” in the fact that it was not the family doctor but the midwife who reportedly told my parents that she believed their baby boy had PS. True, there are several possible causes of infant vomitting, but it seems many surgeons will not even try to diagnose PS, and so resist ordering tests until all other possible diagnoses are eliminated… by which time the baby may have been damaged and days of deep distress added to the parents’ load.
Judging by the many reports online, PS babies all-too-often get to a very distressing and extreme condition before their PS is diagnosed. There may well be some “unspoken history” in the fact that it was not the family doctor but the midwife who reportedly told my parents that she believed their baby boy had PS. True, there are several possible causes of infant vomitting, but it seems many surgeons will not even try to diagnose PS, and so resist ordering tests until all other possible diagnoses are eliminated… by which time the baby may have been damaged and days of deep distress added to the parents’ load.
Because of this, parents who suspect their baby may have PS are well advised to do some very important “homework” to help their doctor decide on the correct diagnosis as quickly as possible, and to help press their case if that becomes necessary.
1 Read what’s on the web or in baby-handbooks about infant PS,
2 Keep records of your bub’s doings (in and output, alertness, etc),
3 Use social media to compare notes with parents with a PS experience, and
4 Have your partner or a close friend support you rather than face a doctor alone.
This will empower parents to if necessary confront their doctor or ER staff with hard facts. All parents can become unnecessarily anxious, but usually a mother knows very well when her baby is losing weight and condition, and can sense when this has become serious. There are far too many stories on the web of parents being brushed off with, “Doctor knows bes t”, “All babies vomit”, or “You’re just a typical over-anxious (or: first time) mother”.
t”, “All babies vomit”, or “You’re just a typical over-anxious (or: first time) mother”.
Is it any wonder that there are so many stories on the web of parents despairing of their doctor(s) and taking their dying baby to the local hospital’s Emergency Dept? There, to add insult to injury, it seems to be typical that they are told: “If you had brought your baby in any later, (s)he wouldn’t have made it through the night.”
This workmanlike guy deserves pride of place here: the German Dr Conrad Ramstedt doesn’t look like an eminent surgeon when judged by today’s dress codes, but back in 1911 he discovered and in 1912 (over a century ago now, yay!) he published the simple remedy for projectile vomiting. And … he’d discovered it partly by accident, partly through good observation and thinking. One of my posts is about this (and there are several more about this pioneer’s impact: find them using the Categories or Search box).
Together with millions of others, I owe my life to Dr Conrad Ramstedt and am deeply grateful to him. Without my early op I wouldn’t be here today, let alone writing this!
Another and more distinguished looking photo of Dr Ramstedt. He started his medical career in the pre-World War 1 German Army. From what I have learnt elsewhere, the scar on Dr Ramstedt cheek is likely from the bizarre university entrance rites prevalent in Germany at the time. To gain entry to a student fraternity, students had to duel in pairs to demonstrate their manliness and bravery. Or rather, they would stab at each other at arm’s length, aiming to scar their opponent. The duellers’ body and arms were protected, but they would go through the rest of their life with an ugly facial scar.
“What a man!” But consider: Is what some “indestructible” young people can get up to nowadays any less crazy?
Well, the surgical technique launched by Dr Conrad certainly tested the bravery of countless parents and babies, and I wear one of those badges!
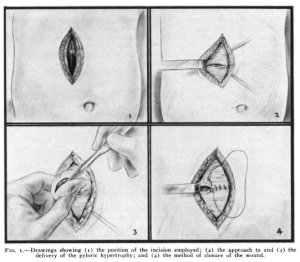
 This 1950s series shows how the Ramstedt pyloromyotomy for PS was (and sometimes still is) done, by open surgery.
This 1950s series shows how the Ramstedt pyloromyotomy for PS was (and sometimes still is) done, by open surgery.
A wave-like stomach contractions (peristalsis)
B projectile vomiting entire feeds (without bile)
C infants restrained and kept warm for surgery (past practice)
D cross-section of the thickened pyloric ring muscle –
E which is cut down to the inner lining –
F of the entire pyloric passage –
G and the split muscle is forced to open wide to allow the pyloric passage to open.
H The thickened and closed pylorus lengthwise
What these sketches don’t tell us is that giving a general anesthetic to babies was primitive and risky until at least the 1960s, and because of this it was often avoided until the late 1980s. This has had lasting effects (psychological issues incl. PTSD) on some of us who had infant surgery before the 1990s. More about this below.
My PS was remedied in the Netherlands in 1945, and my research tells me that at that time only a very few babies were given full anesthesia. Others received a sniff of ether or nitrous oxide (laughing gas) at the most baby-disturbing stages of the procedure. The heart and lungs of infants under 2 can react dangerously to anesthetic gases, and few doctors had the skill to put babies to sleep safely. Pediatric anesthesia as a special skill developed only late in the 20th century.
Judging by most reports of the time from the Netherlands but also Britain and North America, I was most likely tied down, perhaps given some local anesthetic injected around the incision site, and perhaps a sugar cube to keep me distracted and quiet (or try to?). The above illustration shows the tiny patient strapped down and wrapped up tightly to stop it squirming and straining, to keep it warm, and to help minimize surgical shock.
Some babies not given a general or light anesthetic were intubated anyway. They were given a paralysing drug (curare) to keep them from screaming and writhing with the pain of the surgery and had a breathing tube pushed down their throat to keep them breathing. Parents were never told the details, and of course my mind doesn’t remember how my operation was managed, and I’m sure prarents were never told (or wanted to know) the details. But as for my body (or “pre-verbal”) memory… who knows? More about this below.
Pyloromyotomy (splitting the pyloric muscle) has become the favourite operation of many surgeons: it is simple, quick, doesn’t remove anything, and is usually almost immediately and obviously effective, allowing the stomach to pass milk on to the next part of the gut (the duodenum or first part of the small intestine). Just a very few hours after the surgery the baby is usually able to take and keep down some milk – and fear-struck parents are instantly transformed into mightily relieved parents – with the surgeon getting the hugs and kudos!
In the past surgeons were trained to disregard the clear signs of great distress during infant surgery, as still happens today with some or many circumcisions. When only a very few surgeons in large hospitals had the skill to give a baby a safe general anesthetic, the rationale was, “However we do it, we’re saving this baby’s life… the parents won’t know or even suspect the details (nor would they want to!)… but they are always grateful to have their baby back alive and repaired, and no doubt one day their little one will be a healthy and thankful survivor too!”
 Specialist pediatric anesthesia started its development only in the late 1940s, and its spread and use grew only very slowly. Meanwhile it was convenient and generally taught and believed that babies don’t remember pain and (anyway) are not affected by it – until a 1987 study by Dr K J S Anand showed conclusively that neither of these two mantras is correct.
Specialist pediatric anesthesia started its development only in the late 1940s, and its spread and use grew only very slowly. Meanwhile it was convenient and generally taught and believed that babies don’t remember pain and (anyway) are not affected by it – until a 1987 study by Dr K J S Anand showed conclusively that neither of these two mantras is correct.
And so it has only been over the past 30 or so years that it has become almost standard practice that all infants are given a general anesthetic for any surgical procedure, and local pain control is often included for so-called “minor procedures” such as circumcision.
My op was done just like the above drawings show. A vertical incision (in the midline between the navel and sternum, or to the right of midline) was the standard for PS surgery until the oblique (or Kocher or subcostal) incision (angled under the right ribs), and the transverse (horizontal or straight across) incision were promoted, starting with the USA in the 1930s. and becoming the most commonly used for many years.
A small incision around or in the navel (circumbilical) was introduced in 1986 and has proved popular and far less disfiguring. Since the turn of the century, minimal access surgery (MAS) has been gradually introduced for many kinds of first adult and then infant surgery. MAS for a pyloromyotomy gives access to the pylorus via three puncture wounds and instrument probes – and now sometimes just one pathway through the umbilicus. Although MAS has developed and grown in use since 1990, “open surgery” is still used in about 40% of PS cases – sometimes if the pylorus is found to be very large, but it seems mostly by older surgeons too busy or insensitive to adapt to current expectations which may require learning some new and more considerate and cosmetically preferable skills.
There have been many studies of the pros and cons of open vs MAS PS surgery, and the several techniques all remain alive and well. MAS comes with a longer learning curve and slightly more frequent complications, but less post-operative pain, medication, and hospital time, so that the benefits and disadvantages are about equal. The Tan-Bianchi umbilical access similarly has several advantages and disadvantages. And so the advocates of each surgical technique continue to give passionate weight to their preference!
All surgery happens against a background of professional disagreements and medical hazards. Finding the drawing above here prompted me to discover the buried transverse (or horizontal) scar under my 9 cm vertical scar (illustrations 2 & 4 above here). The buried scar seems to be at least 10 cm across.
Some surgeons believe (and others reject this) that two cuts at right angles reduce the risk of the wound rupturing when the baby flexes or cries while healing; this seems to some (only) to be a hazard with the vertical incisions. The transverse incisions are claimed to reduce the risk of wound rupture although the published statistics do not reflect this.
Another internet drawing of what happens in a pyloromyotomy, the medical term for PS surgery. The thickened muscle band around the stomach outlet (left pic) has become 1-2 cm long, whitish, and very hard (typically like cartilage), blocking the passage of everything. It is slit and then prised open length-wise down to the mucosa, the inner lining of the passage, but keeping this passage intact is of course vital: any leak must be recognized and repaired before the wound’s closure. There are several graphic videos showing a pyloromyotomy on YouTube: the one by Dr Wealthy shows the simplicity of the procedure as well as the care that has to be taken to avoid collateral damage that can quickly lead to death.
Another photo from the web – this carefully placed little gash through the overgrown muscle is what saves almost all PS babies today from a slow death by dehydration, starvation, and organ failure. This is the gist of the PS fix – the enlarged pylorus muscle has been split open wide but the lining of the gastric passage is carefully left intact. Bring on the food! Yay!
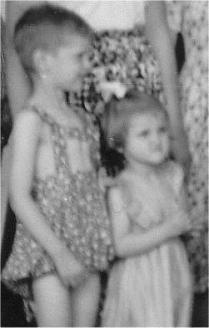
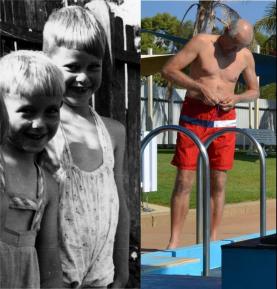
Like many PS babies I flourished after my op! My stressed-out Mother’s milk could get through at last. A simple but effective fix. Just look at how Fountain Fred became Flourishing Fred in the 4th pikkie below here.
 Recently (2023) I have found the only record I have ever seen of my PS story. I remember my parents having my weight chart in their dresser drawer and assumed they had thrown it out in their last years. How good to find it during yet another search of their papers! It shows a solid weight gain during my first 2 weeks, followed by an increasing drop to below my birth weight during my second 2 weeks. (I’m Free, my brother is Henk.) And then: up, up, and away! Whooppee! My pylorus had learnt a severe lesson: it seems it was so keen to avoid further punishment that in all my subsequent days it obligingly let my intake pass through very quickly – which has allowed me to eat as much as I like without a weight problem. How good is that!
Recently (2023) I have found the only record I have ever seen of my PS story. I remember my parents having my weight chart in their dresser drawer and assumed they had thrown it out in their last years. How good to find it during yet another search of their papers! It shows a solid weight gain during my first 2 weeks, followed by an increasing drop to below my birth weight during my second 2 weeks. (I’m Free, my brother is Henk.) And then: up, up, and away! Whooppee! My pylorus had learnt a severe lesson: it seems it was so keen to avoid further punishment that in all my subsequent days it obligingly let my intake pass through very quickly – which has allowed me to eat as much as I like without a weight problem. How good is that!
One minor mystery remains unresolved: one of the few things I remember overhearing in my childhood was that my PS surgery had happened at 10 days. It seems that was about when my story started.
A bit more about my parents and me. This is one of my first photos (and it’s very grainy) of Mum with me. I was born just after the Second World War ended; Mum and Dad had endured a 7 year engagement due first to the Depression and then the WW2 German occupation of their country. Then, 10 days after my arrival (and it seems after some troubling and damaging delay, as mentioned earlier) they had had to hand their firstborn over for what by today’s standards was rough and ready surgery to remedy my uncontrollable vomiting.
 This was followed by a time of quarantine: total separation in hospital from my parents because of the danger of infection (2-3 weeks was the norm). The first antibiotic (penicillin) had been developed by Drs Fleming and Florey in 1941 and became available only in 1944 and then only to help WW2 troops. It was not until the needs of the military had eased in 1946 that infection control became a far greater reality in civilian hospitals.
This was followed by a time of quarantine: total separation in hospital from my parents because of the danger of infection (2-3 weeks was the norm). The first antibiotic (penicillin) had been developed by Drs Fleming and Florey in 1941 and became available only in 1944 and then only to help WW2 troops. It was not until the needs of the military had eased in 1946 that infection control became a far greater reality in civilian hospitals.
So, every day while Dad worked Ma had to travel 32 km (20 miles) to the nearest city hospital (in Leeuwarden) by steam train to deliver some more breast milk for me. I have learnt that infection control meant I could not be breast fed for several weeks, with then unforeseeen effect on maternal-infant bonding that bedevilled Mum and me throughout our lives. I have learnt that the breastmilked delivered to the hospital was poured into a common receptacle, something else that probably wouldn’t happen today. These must have been fun times for Mum and Dad. Surgery and hospital care were certainly rugged and rudimentary in the 1940s and for years after this. And thanks to the web and email, in recent years have I put the pieces together to understand why my parents refused to talk about any of this.
But here’s the good news: I survived and flourished. Half a year after my operation (and probably already at half a month) I was looking very healthy, thank you (if still not very happy). This is quite typical: many PS babies quickly make up their weight loss and go to the top of their percentile range.
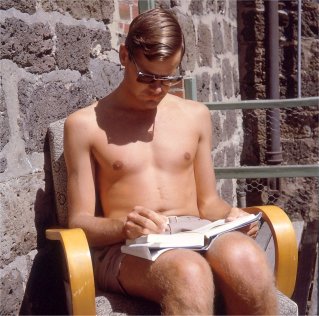
The next page of my story started in April 1951 – it was my “dawn of consciousness”. I’m now 5½ years old, and here’s another fuzzy old photo. This one shows not a sign yet of the trauma and manic phobia I would start to sense during the year ahead, when I came to fear anyone seeing and asking me about the (then) 7 cm (3 inch) scar down my middle. I was quite happy to pose for this April 1951 photo (as many under 6’s do) happily flaunting my PS scar, nicely framed!
Mum had made her (then) 4 kids cute swimsuits in several sizes like the one I’m wearing. They were of a standard design in those austere post-War times – I’ve seen lots of them on photos from that era. To provide vital cover but to save on material you can see they typically had a neat window – which in my case nicely framed the top half of my belly scar!
Now here’s the rub… Not only women have self-image issues: some of us guys too take years to stop hating things about our nature and our body that make us feel marked, different, or damaged. My temperament didn’t help; I’m such an earnest, introverted and perfectionist type. By age 6 years (as is common) I had become self-conscious and obsessed about the in-your-face Frankenstein-like little scar that marked the stomach surgery I didn’t remember or choose even though it had saved my life.
What triggered the change?
After my family’s migration to Australia, my parents hosted a stream of newly arrived Dutch settlers while they were looking for a job and a place to live. Our home was a virtual guesthouse, thankfully without any of the terrible events we hear about only now. With 4 children plus guests, plus a husband often home very late from his work (or away for a week of country-NSW pastoral visits), my mother often drafted the house guests to get her 4 under 6’s through bath-time – which in my case became much dreaded.
“Ah! What’s that you’ve got there?”
(Quickly folding my arms and blushing…) “I don’t know!”
“OK then! I’ll ask your mother.”
A little later I would hear a whispered conversation in the kitchen. I would fume inwardly over my mother who always answered my question with, “Oh, you were a bit sick and the doctor did that to make you better.” Or, “I’ll tell you later some time”. Which of course never happened (I’m not the only one who procrastinates over difficult conversations).
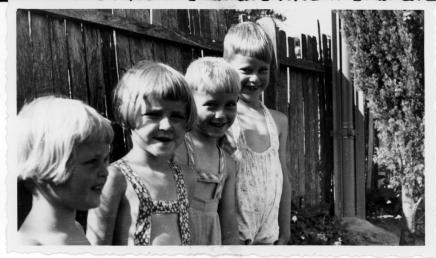 Mum certainly sensed my inner pain, however, and responded as best she could – knowing what little people knew in the 1950s about parenting and child psychology. She made me a special new swim suit without the window frame but instead a rather unhip even higher waist than her earlier design which my brother and older sister are now wearing. I look very pleased with the new gear, don’t I?
Mum certainly sensed my inner pain, however, and responded as best she could – knowing what little people knew in the 1950s about parenting and child psychology. She made me a special new swim suit without the window frame but instead a rather unhip even higher waist than her earlier design which my brother and older sister are now wearing. I look very pleased with the new gear, don’t I?
But this only delayed the issues I would have to deal with.
At this time I also started school with all of its challenges, and with school the learning of English – and facing other unavoidable situations in which “that thing” became an object of curiosity that I couldn’t deal with. My self-consciousness dawned big-time!
 I wish now that my parents had helped me to understand and try to motivate me to “own” my truly life-saving story. Although I didn’t remember any of it, that closed chapter had clearly started to trouble me – and they certainly noticed that.
I wish now that my parents had helped me to understand and try to motivate me to “own” my truly life-saving story. Although I didn’t remember any of it, that closed chapter had clearly started to trouble me – and they certainly noticed that.
Only in recent years have I realized that there is so much reason to be thankful to God, my doctor and my parents that I –
* w as born in a time and place that allowed me to survive, albeit with an markedly imperfect body and some lasting effects;
as born in a time and place that allowed me to survive, albeit with an markedly imperfect body and some lasting effects;
* will always live with a scar which although eye-catching and gnarled is smallish compared with the scarring, disabilities, and body and/or soul damage with which countless others live, often with great courage;
* am reminded daily of the fact that all of us humans struggle in various ways with our creaturely brokenness;
* feel proud of being marked with what represents a lifesaver and a small but important snippet of surgical history;
* belong to a worldwide community of people with a PS story to discover, tell, explore and share; and
* have learnt from my own painful experience that many others live with closed life-chapters that can distort and even poison their freedom, inner happiness, and relationships.
But… not so fast!
During my school years I showed all the signs of PTSD, albeit to a fairly minimal extent and mostly in private. In those times the word “trauma” was hardly heard and the term “PTSD” was yet to be born. Although it was recognized that many soldiers suffered from “shell shock”, everybody was told and forever recited the mantras that “time heals everything”, “you’d better get over it”, and “there’s always somebody who’s worse of than you are!”
Sadly, as we have now learnt, it doesn’t usually work that way. I grew up in a secret world of
– self-obsession (no selfies then but I’m sure I wore out a few mirrors),
– self-injuring (I learnt a lot and am thankful I did myself no great harm),
– re-enacting my operation in child-games and alone, and
– searching libraries for anything to explain my scar and what caused it.
I discovered that I was fearful of especially doctors but also of anyone I regarded as authority, and increasingly became a rather sullen lonely lad, passive-aggressive, and internalising my anger.
 From a young age I loved the coast. Swimming has always been my favourite form of exercise and relaxation, but at the beach and pool in those “carefree” years of childhood and youth I never felt free to relax and enjoy myself except when submerged in the water. Here I am (on the right) hugging the flotation device with my brother and sisters.
From a young age I loved the coast. Swimming has always been my favourite form of exercise and relaxation, but at the beach and pool in those “carefree” years of childhood and youth I never felt free to relax and enjoy myself except when submerged in the water. Here I am (on the right) hugging the flotation device with my brother and sisters.
 Out of the water I would keep my arms tightly folded or tugged my shorts or swimmers up to just under my chest, even higher than this unhip looking football coach. My frustrated Mum kept telling me how ridiculous this looked, but I didn’t really care: I was phobic and nobody could get near helping me about that.
Out of the water I would keep my arms tightly folded or tugged my shorts or swimmers up to just under my chest, even higher than this unhip looking football coach. My frustrated Mum kept telling me how ridiculous this looked, but I didn’t really care: I was phobic and nobody could get near helping me about that.
Although I’m a “hot body”, I would never go without a shirt, even at home or on Sydney’s typically hot or steamy summer days.
When people asked what “that” was on my belly, or what my scar was from. I also made such a fool of myself: I denied my belly was unusual, and then pleaded ignorance about what “it” was. I couldn’t even answer the school doctor – although if he’d read the form my parents would have filled in he would have known! As much as I could, I avoided phys ed classes, sports and overnight camps which involved changing or showering in public, and my heart raced whenever I heard any of a short list of words: doctor, hospital, operation, stitches, scar…
During my late teens and years of courtship I knew my old way would no longer hold, but it took me several years (yes, really!) to summon the courage to tell my best friend and future wife about my PS and scar – only to find that they were (but of course) no big deal to her… I’ve learnt that is typical also! “Chicks dig scars!” And besides that, she told me of a niece who had had the same condition and operation – and as I have discovered, a similar scar too.
But even during our honeymoon this pose shows how careful I was about showing my pockmarked belly to the world. I had survived something that used to kill most babies who had it, but it’s taken me many years to feel as free, proud and grateful to God and my family and friends as I do now.
 “Scar shame” is feeling embarrassed by the furtive glances and curious questions many of us PSers get when we aren’t covered up at the beach, gym, changerooms or in front of a camera. It’s avoided by wearing a shirt or top, and failing that by folding our arms or posing strategically. LOL
“Scar shame” is feeling embarrassed by the furtive glances and curious questions many of us PSers get when we aren’t covered up at the beach, gym, changerooms or in front of a camera. It’s avoided by wearing a shirt or top, and failing that by folding our arms or posing strategically. LOL
“Scar shame” doesn’t worry everyone, but I’ve learnt that I am far from alone in having struggled with it for many years. These two web images of PSers make that obvious!
I well remember the horrible hot flushes and racing heart that underlined the state of my inner self whenever I felt “discovered” or “exposed”.
It would be several more decades before I felt I had largely succeeded in putting my scar shame behind me.
So, “get over it” I did!
There is hope for everybody who struggles with “scar shame”.
However, I still feel inner anger when I read surgeons (esp. of the pediatric genre) who dismiss “cosmetic considerations” when defending their established practice of doing open surgery when it’s not the only option.
And although I realise that we can’t judge past attitudes by today’s knowldge, it angers me that so many of my contemporaries (and somewhat younger) have huge and very disfiguring scars from their PS surgery compared with mine. PS surgery was done by general surgeons as pediatric surgery only started, and slowly, in the 1950s. If an old-time general surgeon had big hands or a careless attitude, the rule was: “Give yourself plenty of room to work, you’re doing this only to save lives.”
Despite being a 187 cm (6’1″) beanpole and now watching my weight, I’ve added a bit of flab in recent years and my scar has become indented, which is a common look. It’s also become clear that adhesions have also glued the scar to my innerworks. I’m thankful that this has not caused me any further trouble, which is sadly not true for all Py babies as they grow up and go though life.
I’ve learnt a great deal about my PS story and how I’ve reacted to it – but almost all from web-based sources and interactions.
Sadly, my personal story, what only my parents could have told me, will remain an almost total blank. Their lips remained sealed, sadly to their graves. In their times, medical matters and unpleasant stories were usually not talked about: their terse mantra was, “the doctor did that because you were a bit sick.” We would talk about this “later”. In the endless mean time, I should “stop acting in such a silly way” (trying to hide or deny my scar). I wish now I’d had it in me to challenge them about all this before it was too late! But that was not my way.
Aspects of my early surgery will always remain a mystery to me, although I understand much more now than what I learnt from my parents – or what they knew. Here are some of what I have learnt from research and networking with others –
1 Infant surgery pain control was a closed subject until the late 1980s.
2 Inadequate pain control was once common and could affect a baby throughout life.
3 The effects of lengthy hospitalization, often in isolation, were long not understood.
4 The effects of maternal deprivation of breastfeeding was also long not understood.
5 The very early starvation PS babies often suffer can affect brain development.
6 Parental nurture and the cultivation of trust were also long not understood.
7 The effect of infant trauma on parents and children were also long not understood.
Recently I had a brain CT scan as part of a medical diagnosis. My neurologist took me through my brain, looking for abnormalities. Layer by layer, she explained the geography of my head, and I was amazed how symmetrical and tidy my brain looked! But that was until she stopped at one cross-section which showed a substantial dark area, only one one side. “Oh, you’ve had some trauma there,” she commented.
I was intrigued but didn’t connect until my wife and daughter raised her comment on the way home.
“That sign of trauma, I can only think it was from the operation you had for PS, or the trauma of all that!”
I could only agree, and researching this soon learnt that non-verbal memories and emotional trauma can show in the brain.
Which of the above 7 aspects of my PS story may have caused this trauma I can only speculate, of course, but with the physical proof so obviously there, I feel strangely reassured that what I have lived with, researched, and suspected for most of my years is not pure imagination.
I am telling all this in some detail to encourage greater awareness of the many aspects of infant surgery, and not only as I experienced it. With countless parents I want PS to have a much higher profile among medical personnel (notably GPs and pediatricians), and among new parents and their supporting family circle. I want there to be no more pediatric surgeons who brush off “cosmetic considerations” as irrelevant to infant (or any other) surgery.
I also want every parent of a PSer to be able to do much more today to help their child to understand, embrace and be able to talk about their story, especially if their growing child struggles to understand and “own” their scar and its genesis.
This photo from a German medical website is very special to me. The father on the left has almost a clone of my scar, and his son has had a laparoscopic PS operation.
This image was posted on a German website to show the progress PS surgery has made since 1980 when a baby’s belly was still routinely slit open and then sewn up like a football with big black threads… without much thought being given to the tiny patient’s self-image and self-confidence in later life.
I have recently learnt that the railway-track-like scar (which I share with the father above here and many other older folk) is the result of a wound being closed with retention sutures. Sometimes these sutures were grotesquely large. This is a subject of its own, but these sutures were chosen to support a midline wound so that it would not rupture (given that our front middle area has few blood vessels and little muscle). Having seen some results of midline surgical wounds reopening, this is not an imagined hazard.
Usually today, such sturdy sutures are buried in the wound, and small staples or buried stitches or even just strong adhesive tape holds the surface skin layer together while the wound heals.
 In the past even infant wounds vulnerable to rupturing were closed with sturdy threads taken through the skin and underlying muscle, which were then drawn tight, tied, and then left for a week or two. They would cut slowly through the baby’s tender skin, leaving the large and elongated pockmark stitch scars I have. This was done as a precaution, especially when the baby’s condition was weak. It would save time, which was just as critical as avoiding rupture when it was not safe to fully anesthetise the baby, and when the infant was conscious and suffering throughout the surgery.
In the past even infant wounds vulnerable to rupturing were closed with sturdy threads taken through the skin and underlying muscle, which were then drawn tight, tied, and then left for a week or two. They would cut slowly through the baby’s tender skin, leaving the large and elongated pockmark stitch scars I have. This was done as a precaution, especially when the baby’s condition was weak. It would save time, which was just as critical as avoiding rupture when it was not safe to fully anesthetise the baby, and when the infant was conscious and suffering throughout the surgery.
So retention sutures would help to prevent wound rupture if the baby cried and strained during the first post-op weeks. Midline vertical wounds cut through the blood-poor linea alba and are said to be especially prone to rupture. Today when retention sutures are used (almost always for ailing adults) bolsters or tubing (as shown) is used to keep the sutures from cutting through the skin.
Wound rupture is less common today, and retention stitches in a baby are almost always buried in the wound. Stitches closing the skin are usually cleverly buried and may leave some unevenness but no visible scars.
Quirkily intriguing to me is that not a few PS scars I have seen, including the German one above and my own, have a little crater somewhere along the incision line: I wonder if a drain was sometimes left in the wound?
In recent years, at least the younger medical community is becoming aware of the importance of doing infant surgery in such ways as will leave the least possible visible damage. Sadly, I have noticed that some “old hands” still ridicule any consideration of cosmetics, and some medical people even promise that the wound will slowly disappear and certainly not grow with the baby. Wishful thinking… false comfort.
However, we can all be grateful for the slowly growing recognition that infant surgery can leave some (or many perhaps) of its patients vulnerable to various psychological and emotional challenges. Yet this awareness seems to be growing very slowly indeed. Interestingly apart from the USA where therapies of many kinds seem to flourish more than anywhere else, the recognition of the potential damage caused by infant surgery without pain control seems to be strongest in the Netherlands – where it all began in my story!
As mentioned, during the past 15 years the surgical repair of PS has increasingly b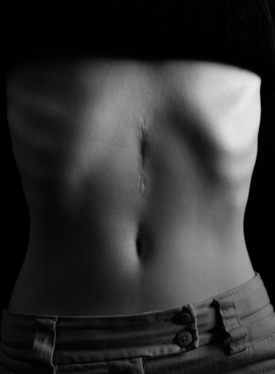 een done via 3 2-4 mm laparoscopic probes. And when a surgeon chooses to work through an open incision, the stitches that close the wound are almost always buried to leave a much tidier scar, as this beautifully captured image from the Life Lines blog shows.
een done via 3 2-4 mm laparoscopic probes. And when a surgeon chooses to work through an open incision, the stitches that close the wound are almost always buried to leave a much tidier scar, as this beautifully captured image from the Life Lines blog shows.
Although laparoscopic PS surgery doesn’t leave much damage at first, by school age the probes often leave scars that have become navel-like pits on the abdomen: as someone has commented, “My belly looks as if it’s taken a shrapnel hit”.
Another old discussion centres on whether almost all PS needs to be treated surgically. Reports from several developed but non-English speaking countries show that over 80% of PS babies will actually respond to medical treatment with the drug atropine (or similar) which relaxes the pylorus muscle until the baby’s growth takes its own care of PS. Although medical drug treatment takes a little coaching of the parents and a course of several weeks, it is safe and non-traumatic for both the parents and the baby… and the surgery option can always be taken up if necessary.

Ranitidine used to be favoured to reduce gastric acidity. In 2020 its possible link with cancers resulted in it being replaced with other effective drugs.
One of my blog’s many “messages” is that medical treatment should be the first option offered for all PS babies older than 3 weeks. It will very likely avoid inflicting the trauma of surgery on the parents and their little one. If unsuccessful, surgery remains as a safe second option. In countries with this policy, it is just as safe as the surgeons of the Western world’s preference for the scalpel. In the medical world it is only the brave who dare mention the otherwise well-known observation that in their empire, the surgeon rules!
Now, welcome to my Blog! Please consider leaving a comment below here, or something of your PS and/or infant surgery story.
If you’d prefer to email me, the “About me” and “About this blog” pages to the left of the tab for this “page” enable that.














Dear Dr. Fred,
You know me – honest. I have just read your blogs. Many many congratulations. I have been invited to submit 48 plus pages for a book to be freely published on pyloric stenosis of infancy..
Have been looking for an arresting opening piece and I can think of no better way than to use your words and experience, and make it personal.
Would you be interested in a free publication as a joint author with me?
48 pages A4 is quite a lot. You could do the history from a personal standpoint and I could concentrate on the cause of the condition with a plea for the use of IV ranitidine. Your photos are simply great.
Shall send you the email to me inviting me to create the book.
Best wishes,
Ian Rogers FRCS,FRCP,PGMCEdu
I am really excited about these 48 pages to be published. How thrilling! Can’t wait! About “My Story,” wonderfully told. And yes, the pictures add so much. One thing I’m curious about is your statement “medical treatment should be the first option for all PS babies older than 3 weeks.” Why 3 weeks? Can’t the treatment begin earlier? I love the new format of your site, btw. It’s clear that you put A LOT of thought into it, which paid off. I’m so proud of you, your blog, and your latest thrilling opportunity to publish, with a renowned surgeon and researcher, your very important and beautifully told story.
I am very grateful to Dr Ian Rogers for his kind invitation to include some of this my personal story with his contribution to a forthcoming book about pyloric stenosis.
Thank you, Ian and Wendy, for your commendation of this Page of the SIS blogsite.
Wendy, my reading has taught me that because medical treatment takes some time to take effect, there is a higher risk of its failure when the baby is very young, with minimal reserves. And if it then becomes necessary to switch to the second option, the infant would likely be in a very poor condition to withstand surgery.
In answer to the three week wait question – symptoms and signs usually take take 3 weeks from birth to develop – hence diagnosis usually made at this time and treatment can only then begin.
Ian
Thank you, Ian! With regard to my pyloric stenosis experience, at 26 days old I weighed 4 pounds–down 2 pounds, 7 ounces at birth. At 3 weeks, I’d already lost quite a bit of weight. Do symptoms of some PS babies appear earlier? Fred, have you heard of symptoms appearing earlier? You were operated on at 10 days old, right? So doesn’t it vary? Thanks ahead of time for the clarification.
Yes, symptoms can start to appear from almost the first day, even with premmies. The great majority of cases show between 3 weeks and 3 months, and mothers are now advised to continue breastfeeding up to age 6 months if they wish to reduce the risk of their baby having PS. There are even a few cases documented as having been diagnosed later than this although it’s then asked if these babies showed earlier signs.
Thanks so much for this clarification, Ian. Your depth and experience show!
I have just started looking into PS related problems as my son, who is now 7, has been having a very sore stomach for the past 2-3 months. He had acute PS and surgery as a baby. His history is that he was born 5.5 wks early (induced for a blood disorder reason) and he spent 3 weeks in hospital with no real sign of vomiting. (Incidentally my first born son was a very sicky baby and looking back it is quite likely that he had mild PS although he never had any malnutrition issues) Once he was home within 2 days he suddenly began being sick and within 24 hours it was apparent that he hadn’t kept any milk down. Fortunately we had a follow up hospital appointment (for routine blood tests); as the GP wasn’t prepared to act any quicker, we stayed in the assessment unit and he had a urine bag put on but he went another 12 hrs without passing any urine before the doctors took real action. They put him on IV fluids about 2 am after finding how knocked off his electrolytes were when his breathing began to become intermittent! (very scary) The next day he had a barium x-ray which confirmed the diagnosis and he had surgery that day (keyhole through his belly button). He made an instant recovery and I thought nothing more of it until now. He does seem to have pain pretty much constantly in his tummy, this last 3 weeks have been gradually getting worse so the information in your pages has been very helpful. He is going to be started on anti acid medication which I hope will help, but I have taken on board the issue of the gastric bacteria and will keep that in mind if he doesn’t pick up soon. Interestingly the GP said she didn’t know if there was any link to his PS surgery but she was keeping an open mind.
I feel a bit more informed and will take a lot more notice of my little boy`s complaints about his tummy now !!
Thank you Sara for telling us something of your son’s story. Thanks also for your feedback: I always get a buzz when I find that people have been helped by the information I pass on here.
You have a good grasp of what you and I could know without actually running tests. Keep in mind also what I have written about adhesions: from the stories that have been told here, a 5 year old was the youngest to have surgery to relieve obstructions caused by PS surgery… That would not be done so young unless it was very necessary; I do hope your son doesn’t have to travel that road.
My best wishes as you follow through on your son’s troubles: this needs to be diagnosed and dealt with. It would be valuable if you let the readers of this blog know how you go.
Hi Sara, I’d certainly like to know how things turn out for you, your son and your family. I’m sending warm heartfelt wishes for a good resolution. Please keep Fred and the blog posted.
Very interesting. I too had ps and had an op when I was two weeks old.
My scar runs right down the right hand side of my stomach, a big scar. Recently I was in hospital with a gallstone stuck in the bile duct of my liver. Surgeons tried four times to put a camera down with a tool to remove the stone. But the way my ps op was done in the ’50s they can’t get near the bile duct to remove the stone. Part of my stomach is cut off and has made it impossible for them to remove the stone that way. I was in three different hospitals and the 3rd one was King’s College in London. And I had one of the top liver surgeons (Mr Philip Harrison) and not even he could do this.
Elaine
Thank you for giving us some of your ps story, Elaine. In my reading for this blog I come across people quite often who have gall bladder blockages after they’ve had the op for ps. Sometimes the trouble hits when they are only in their early 20s – so perhaps you were (a bit) lucky. The ps operation causes adhesions (I’ve written about them several times here), which as your doctors found can sometimes choke off various organs. Some of these people were told after their gall bladder surgery that there was nothing wrong with their gall bladder, but that the bile duct (the hose from it to the intestine) was blocked by adhesions. I hope you are over the problem now.
I feel so enlightened having just read your pages Fred. I am 27 and was treated for PS at around 4 weeks old. My twin brother also had the condition. Bryn (my brother) has never had any problems with his scar or putting on weight. I, however, have quite severe discomfort when exercising and also suffer with acute nausea if I am too active after eating. As an adult, I have remained the same weight for a long time, and little seems to change this. I stopped eating dairy about a year ago, and since then, I must say that the discomfort has eased, but this may just be a lactose intolerance. It seems very hard to tell what correlates with the condition or not!
For a long time, I was extremely self conscious of my scar, and would never wear swimwear or cropped clothing. Thankfully, I no longer care and am quite proud of my scar and the story it tells. My scar very large and knotted, whilst Bryn’s is no more than an inch and very neat. GP’s in the past have said it is likely I may have trapped nerves in the scar which may be causing the discomfort, but it feels deeper than that. Reading your story, and the others who have shared theirs, has really helped me get some clarity over the long term effects of the surgery.
Thank you for sharing.
Amy
So glad you found your way to Fred’s site! I had PS and have had more emotional than physical long-term effects. In any case, I too am grateful for Fred’s blog and all his work to enlighten fellow PSers.
Thank you Amy and Wendy for your warm and wholehearted responses.
I am so glad that by my writing here others are able to experience the reassurance and affirmation of their own struggles after PS which I did when I first “met” other survivors and continue to enjoy when folk like you share something of their own stories.
Hi Fred,
I just found your blog and I can only tell you this has been a healing experience for me. My story is very similar to yours, It was like reading my own experience with my scar as a young person. I have tried to find information in the past about my scar with no success. This has finally explained so much. I have always had a profound phobia of doctors, hospitals and the like. No wonder!!!! My operation was performed at 3 months old in a very small country hospital (January, 1974) so I cant imagine they used anesthesia. I was very emaciated at the time as the doctors attributed my condition to the poor care of a very young mother. Gratefully, one of the older mothers of the community brought my Mom to the clinic and had a frank talk with the doctor :):) My mom said just as the woman was finishing her discussion with the doctor, on cue — projectile vomiting! I was immediately brought to surgery! How much pride it brings me to read the history of Pyloric Stenosis and I too owe my life to Conrad Ramstedt. Moving forward it now gives me pride to be a part of the history and see how current and future generations will benefit from the advances made. If you would like another picture for records I am happy to send one.
Very gratefully, a big fan, Rebecca
Thank you so much for your affirmative comments and sharing something of your story, Rebecca. It’s taken me many years of searching, reading and reflection to write some of the things I have on my blog, and every now and again folk have responded as you have here: this shows so strongly the confirmation my writing has given you and it also affirms me: I am not unique in a way I don’t want to be, and the scar which has been such a source of pain and hatred is something I now understand and can own with pride and gratitude because of all the good and not-so-good that lie behind it. You have put all this so well in your own words. I’m grateful too for the advances that have brought much change to the way infant PS is often handled now, but there is still much to be done in educating tradition-bound doctors and parents who don’t know the symptoms. Best wishes!
What a wonderful site, and so amazing to see other people’s stories similar to mine. I recognise so much of it. One question – has anyone else experienced weight gain issues in later life, and do you think this can be in any way put down to the PS or pylorectomy? My mum often questioned whether the surgery had damaged my ‘stop mechanism’, since as a child, given the chance, I would eat and eat until I was sick. I still struggle to recognise when I’m ‘full’. I’ve learnt to manage my weight through healthy eating, but it’s just a thought.
Looking at scar revision in the coming months, having recently lost a significant amount of excess weight.
Thanks for your Comment here, Helen. Yes, isn’t it reassuring to discover that what I thought was my private pain (or as I thought, weirdness) is in fact something others like me have also had to come to terms with?
Weight-gain issues are a bit of a puzzle from what I’ve read. If only somebody with a doctorate would do a thorough study on this! On the one side, many report what you do: that their stop mechanism seems to be non-existent and that they can eat until they’re sick (and some even end up puking). On the other hand, we realise many people have “a weight problem” of some kind, so what’s different? It seems the signal – but who can really say there is a difference between us PSers and the others? No wonder a doctor who has just 10 minutes for each patient doesn’t buy into these complexities!
I’m at the other end of the range but with similar questions: my son (age 34) can also eat a chicken without weight gain – as I could at that age. But he and I belong to a strand in my family with tall, lanky frames, few if any weight problems, and a suggestion of gastric issues. Is this linked with PS? The over-acidity that kicks the food along and may cause IBS and gastric ulcers certainly seems to be.
Good on you for looking into scar revision! If your scar is indented, that can be improved a lot. I’d value being kept in the loop here or by email if you go that way. Best wishes.
Hi, great to find this blog, just thought I’d share my son’s (and my) story with you.
My son was born in 1994, a very large, long baby, with a big head! He was an emergency C section but all went well and he was healthy. After about 5 weeks he began to vomit quite violently and was not keeping much of his feed down- frustrating for him, being perpetually hungry, and me, as I was breast feeding!! (I started giving him bottles of formula because I couldn’t keep up). I had read about PS and suspected my son was showing signs of this. At the six week check however, the Dr I saw poo-poo’d my concerns and told me I was being overly worried, probably because I was a first time Mum ! ! I knew my son was ‘not right’ but went home feeling very frustrated, tired and angry at not being listened to. Luckily my mother-in-law was soon to witness my son projectile vomit and she insisted we return to the Dr. By this time my cheerful smiley baby was looking very sad and he was growing quite listless.
This time we saw my regular Dr, and she immediately noted that my son’s fontanelle was depressed, indicating he was dehydrated; she also weighed him and discovered he had not gained any weight. This Dr wasted no time in sending us straight to the local hospital where I had to give my son a barium feed so he could be x-rayed (I think it was, not a scan). Soon after this it was confirmed that yes indeed he did have a pyloric stenosis and would need to be operated on!
All in all quite a traumatic time but I’m glad to say the operation went well and he is now a healthy 20 year old of 6 foot 4 – very tall and skinny, but eats like a horse. His scar is about 2 inches long and barely visible.
The lesson I learned was that as a mum, first time or not, trust your instincts!
Being hungry basically means having lots of acid – thus the hunger is maintained even at age 20. There is evidence of a statistically significant greater birth weight in the Py babies and they often are rather athletic and muscular.
Ian Rogers FRCS/FRCP.
Date: Wed, 27 Aug 2014 17:07:09 +0000 To: irogers2000@hotmail.com
Thank you, Julie, for telling us something of your Py experience. Great to find that after all the upset your son has done well.
Thank you too, Dr. Ian, for your valuable knowledge and experience.
Dear Fred, the indigestion in later life experienced by PS patients is often due to the other consequence of too much acid – a duodenal ulcer, so antacids ought to do the trick.
Ian
I think as a baby I may have had PS and was misdiagnosed … Had an emergency exploratory operation when I was a few months old.. I am 53 now and and all I have read here is so much like my life story… At 14 years old I also had another emergency exploratory and 12′ of gangrene intestine removed…. I can not tell you how many doctors I have spoke to in the past … Not 1 has mentioned this condition to me. Would so much like to learn and share what I have been through.
Thank you for this response, Jim. The readers here and I myself (as obviously deeply interested in the people and issues related to PS and infant surgery) would benefit greatly from knowing more of your story. This sort of information is valuable when shared because it extends and deepens lay and medical world awareness of the issues, and for many of us “going public” or “coming out” with our struggles, lessons learnt and victories is very healing.
Yes, I echo Fred’s encouragement. Bring your story on! Share what you’ve been through so others may see themselves in your story. I, for one, would appreciate it.
Hi there. I was diagnosed a PS baby in 1970. My parents did everything to avoid surgery. Neither of my children inherited the condition – I was most relieved, as I was told for a female to have the condition it would then mean that a boy born to that female would have a 60% chance of having PS.
I am now in my 40’s and are trying to work out a lump in my throat and mild pain in the middle of my chest.
Is there any connection with non-surgical PS babies and later life stomach/reflux issues?
I do occasionally have reflux in the middle of the night, but I am not overweight and maintain a healthy diet.
I challenge I find is that all medical people I have come across have said I could not have had PS because I never got operated on and that it was impossible for me to survive, so I have even gone so far as to question my mother’s word on the issue, wondering if it was severe GERD …
My sister has a severe GERD baby … unless it’s misdiagnosed PS too.
I would appreciate any comment you might have.
Kindest regards
Beth
Thanks for writing in, Beth, and telling us something of your story.
Just a few comments in response to what you wrote and asked.
It is commonly said among doctors that if a baby’s PS is not killing her or him, then it’s pyloroplasty, a spasming but not enlarging of the pyloric ring muscle. While that may be generally true, I have countless medical articles and personal stories on file that show it’s not always so simplistic! But doctors can’t remember all the countless details of their area of knowledge!
Mild cases are ones that are diagnosed by U/S, xray or other means but then treated medically or just “watched” in case surgery is needed. Some of these babies have continued trouble, and some of these are operated on at a later age. I can give you stories if you wish (send me an email via blogsite’s info pages).
The good news (I trust): I have not come across a throat lump and mild chest pain as symptoms of ongoing or adult-onset PS.
The bad news (although I trust you are past worrying): people who had or have PS but without surgery can still pass on the condition to their children. But the risk is between 5 and 20%, not quite 60%!
PS is caused by high levels of a blood hormone that triggers acid release in the stomach, and this is related to both infant and adult PS as well as GERD, IBS, and peptic ulcers. However, many people battle with these but have no PS in their family genes.
We and the medical world still have a lot to learn!
Best wishes.
Thank you for your detailed response. I just know my parents always wondered if they should have allowed the operation given how hard it was for me as a baby, and them as my parents. As I grew up, and seemed to grow out of the condition, I was often very ill and they always wondered if the PS had something to do with it all.
I see from your blog that there is trauma either way for both parents and child and feel very grateful that neither of my children inherited the trait.
I am not sure how to give you an email via blog sites info pages.
I can see you do a good thing on this blog site and I hope and trust that through it comes healing for both yourself and the countless others that come across your site.
You are right – we really know so little medically.
Thank you Beth for your understanding and kind endorsement of what this blog is about.
I was operated on in 1959 for ps, when I was six weeks old. I was 9.5lbs at birth, but by the time my ps was operated on, I weighed considerably less and was severely dehydrated and malnourished – very seriously ill. I have a photo of me taken shortly before my diagnosis and I look like a shrivelled prune. When I was younger, especially a teenager, I was horribly embarrassed by my scar, but I now at the age of 55 love my scar as a constant reminder of how I very nearly died and of how precious life is. I am interested to hear that general anaesthetics were not used – can this be right? That is horrific. Could I REALLY have been operated on with just local anaesthetic? I wonder if this is the reason why I have a horror of “cutting”: I hate knives, scalpels, scissors and have an absolute horror of the damage they can do. The reason that I found this blog is because I am trying to research something I heard years ago on the radio when I was just twelve and travelling in the back of my parent’s car. The radio was on and there was a medical programme. They were discussing the possibility of a link with pyloric stenosis and enlarging of the heart muscle later in life. I asked my parents to explain what the Doctor being interviewed meant, but my parents hushed me and told me not to worry, it was nothing. It has always stayed with me, and particularly since my older brother has been diagnosed with hypertrophic cardiomyopathy, which can be hereditary. I have not found one article which says anything about a link, which is reassuring. So glad I found this post though.
Thanks for sharing something of your ps story with the readers here, Linda. I can relate to a lot of it, and so much of what you mention is quite common to (now) older ps-survivors.
I can reassure you that in 18 years of reading everything I can find online about ps, I have never read of a link either between ps and heart disease. However, ps does quite sometimes come with a list of other birth defects (up to 20% is often mentioned), but if you are not affected by hypertrophic cardiomyopathy, it is likely that (if it is hereditary) it’s stronger in your brother’s genes than yours.
In 1959 pediatric surgery and pediatric anaesthiology were still in their infancy, and using general anesthetic on babies is very different and more hazardous than in after age 2. However, some surgeons report using ether (sparingly) without it causing deaths. There is little on the record, but it seems that local pain control was the standard. There are also several personal accounts from people who were told they were “kept happy” by being given a sugar cube to suck, sometimes laced with rum! Wow! It was then commonly stated that babies do not feel or remember pain, but did people believe this mantra?
Then there was the issue of infection control, which often meant the baby was kept in hospital for around 2 weeks, much of the time in sterile isolation.
My parents like yours never answered my questions and in my earlier life I didn’t have the confidence and skill to challenge that. Reflecting now, I believe they didn’t want to know the details of my op, and that if they did know, they’d rather not tell. So I too had a lot of damage to deal with in my earlier life, some of it continuing. The phobia about cutting you mention is reported quite often. I have written about some of my ptsd-related struggles in my blog, and am always happy to enlarge on this off-line.
Thanks to all for sharing about PS. As a boy of about 10 yrs I had the symptoms and only at the age of 19 yrs I had a surgery done, and unfortunately after 10 days of surgery, it was not successful and a Gastrostomy had to be performed – a gastro jejunostomy (it allows food to by-pass the obstruction). The late Dr EM Barker performed the surgery and also found that I had pyloric stenosis, I suffered for 9 years had a very bad schooling career, but thanks to the Doctor I am in good health and a male adult of 65 yrs with 6 grandkids.
Thank you, Booi, from me too for your post and telling us here some of your story.
PS comes in several forms, and your story is different again from most others I have read. What a distressing a time you have had: all that being very unwell and losing strength and energy for 9 or so years at a stressful time of your life and interrupting your education. This followed by what will have been a major operation.
People who have had something similar write about their deep frustration at the slow diagnosis, unsuccessful alternative treatments, endless tests and doctor visits.
But you have made it through! Congratulations! I do hope that your gastric problems will have truly ended.
Hi Fred thank u very much,I do appreciate your response. Kind Regards. Booi
Sent from my BlackBerry® wireless device
Oh my gosh, B., I’m so sorry for all your pain both physical and mentally. And how happy I am to read that you are now in “good health . . . with 6 grandkids.” You’ve gone through so much. Thank you for sharing your story. I don’t know that I was lucky to have a pyloric stenosis surgery at 26 days old without anesthesia, for I’ve suffered a lot both physically and mentally, but looking back, I am glad I survived. We are a tough group, are we not? I’m glad you’ve come out the other side.
Hi Wendy, thank u very much for the reply, it makes us feel that we not alone out there, due to the surgery. I have to sometimes take antibiotics for the bacteria build up (surgery allows food to by-pass obstruction) – gastrostomy-jejunostomy medical terms LOL
Regards and take care,
Booi Maharaj
Dear Dr. Fred:
Thank you for your fascinating blog and all the information! My older brother (first born) and I are both PS survivors. We had surgery as month-old infants in 1961 and 1964, respectively. Our parents told us when we were growing up that we were very lucky because the doctor who operated on us was the “son of the doctor who invented the operation.” I don’t know if that is true or not, and I never knew who invented the operation until I came across your blog today. We were both treated at a hospital in Jackson, Michigan (USA). Since my parents already had experienced the illness in my brother, when I began projectile vomiting at about 1 month old, they immediately sought treatment — even though they had been told PS wasn’t common in girls. None of our younger siblings (one girl and two boys) had PS.
As for the surgery, our scars are horizontal and have been very faint for as long as I can remember. My scar is just under my sternum and goes for about 15 cm, toward my right side. It seems significantly higher than what I saw on the diagrams and pictures. I have a very slight dimple or two in the scar, but barely noticeable. I believe that my brother’s scar is similar to mine. From what I read of your story and others, I feel very fortunate to have had minimal scarring and no side effects that I know of related to the PS. My brother has had problems with GERD. I believe that those problems started when he was in his 20s.
I am not sure how common it is to have two children with PS, especially a boy and a girl. We are not aware of any other family members with PS. One other point is that we were both breast fed for at least the first couple months (minus the hospital stay!). Since we both developed our PS prior to any significant bottle feeding, I don’t know if that would have been a factor.
Anyway, thank you again for sharing your story!
Best regards,
Sue
Thank you so much, Sue, for your response to My Story; you also have been very informative which I value, as it helps me and all our readers here to appreciate the great variety in our stories about the same condition and technically similar surgeries.
Here’s some feedback…
I find it interesting that at least four countries claim to have discovered the surgical remedy for PS! In alphabetical order these are France, Germany, Scotland, and the US. I may write a post about this one day! In fact I’ve found that each of these surgeons’ approaches and contributions was slightly different. The pyloromyotomy today is commonly named Rammstedt’s operation after the German’s “colorful” discovery in 1912 and publication of it in 1913. I believe the other three developments were earlier, but they didn’t tell their story as well or not publish them at all. Let’s say “the time was ripe””: there seems to have been a widespread interest in finding a less risky procedure for a rather common condition.
The horizontal scar you describe is from a high transverse incision, at the long end of the range long (mine is 9 cm long) but tidy for the 1960s: transverse incisions from just under the right ribs to just above the navel have been and remain the most popular of the traditional open surgeries for PS.
Although the majority of PS cases are single ones in the (extended) family, multiple incidence as in your case is quite common and suggests a hereditary element. I’m glad there have been no other cases. PS occurs with just so many variables: bottle feeding has recently been found to increase the risk, but so many of us were breast-fed; being male. firstborn, Caucasian, and having an anxious mother are all risk factors, but again, there are many who didn’t have any of these ticked boxes against their name.
Your brother’s GERD could be caused by the high acidity which is a large part of what causes PS in babies and is not remedied by the surgery; it can also be caused by adhesions from the surgery and can develop quite quickly – over many years.
Thanks for your interest and taking the time to write. I trust these comments are of some interest to you.
By the way, Sue, I’m just “Fred” and not a doctor! It’s just that my experience of PS has given me a strong personal interest in researching and writing about it.
Best wishes – Fred Vanderbom
HI Fred,
I find all of this very interesting as I have a daughter (now 11) who had this surgery at 20 days old while we were living overseas in South Africa. She has quite the scar, vertical. It looks very similar to yours in fact. It is puckered and pulled. I remember thinking she did not have enough stitches in it when I saw her after surgery. They were thick and black like you described.
Anyways, she has avoided eating since she was a few months old. Even now there are only about 25 foods she will eat. I was wondering if you have ever heard of this connection with this surgery? Thanks. Amy
Thank you for your comment in response to this page, Amy.
It makes me both angry and sad to find that this rather common surgery is still being done by some using a very outdated and now insensitive technique. It’s one thing for me as a 70 year old to wear a museum-piece surgical scar, but your 21st century daughter?
In many years of reading and learning about infant PS, I have come several unusual eating patterns after this condition, but never one like your daughter’s. Several questions occur to me –
1 Could she be showing a family trait here or mimicking (say) dad or mum (as one of my grandsons does)?
2 Can she tell you why she doesn’t eat “exotic” foods? (Taste? Discomfort? Some association or fear?)
3 Because this choosiness goes so far back (“a few months old”) there may well be a link with her surgery. I have read and written often on SIS about the possible psycho-somatic effects of some infant surgery. Although most PS babies soon develop a voracious appetite after their surgery (as I did), others quickly develop reflux, IBS or bloating and need a special diet to minimise this. Some refuse to lie on their belly, clearly due to wound or internal discomfort.
4 Your daughter may now or in a few years be able to talk about her food fussiness with a wise and sensitive parent or trained therapist. I advise against forcing her on this matter. You might raise it with her gently and just occasionally in case she does now or in the future feel troubled by her situation and becomes motivated to deal with it.
Best wishes!
Hi, since I was about 6 yrs old, I suffered with the symptoms of PS; only at the age of 19 yrs it was confirmed and I had surgery done, and 10 yrs later I had to have an Gastrostomy done (Jejunostomy – it allows food to by-pass the obstruction). Ever since I am in good health, I do take a tablet called Creon 10,000 which avoids loose stools whenever required. I am now 65 years old and enjoying my retirement with my family and 6 grandkids, God’s blessings are with us all.
Booi Maharaj. 0834757218
Sent from my BlackBerry® wireless device
Thank you Booi, for telling us here something of your PS story and the relief you have had since your surgery. I heartily agree that you have indeed been blessed by God! You have had few of the ongoing problems that are often reported after jejunostomy, which by-passes the stomach and often causes the problems you mention and others. Thanks for recommending the medication that you have found so helpful in controlling this. Enjoy your retirement and your family – as I am also!
This is very interesting to me. I, my brother, one of my cousins (that I know of), my two daughters, my sister’s two boys, my grandson and my aunt’s grandson all have had ps. It definitely runs in my family. And the “not in girls” was the attitude which held up my and my oldest daughter’s surgery. Now it’s one of the first things they look for in my clan.
I was the one who almost died but the ones following me were checked right away. So that’s nine (maybe more) in 3 generations. In my immediate family it hasn’t skipped a generation.
I was told I was so bad my mom wouldn’t even put me down to go to the bathroom. I’m one of the 50’s survivors, but was never embarrassed of my scar, that I remember.
I would have thought that it would weaken with different genes introduced into the family via marriage. Ah, but no, not at this time.
Thank you so much for your Comment, Shirley. Good friends of ours also have PS well-represented in at least 3 of their generations, but your clan takes the cake! I also have on file internet reports of multiple incidence, but certainly in your part of your family tree, you also beat the percentage of any of these hands down. You didn’t mention any deaths in the past from untreated babies in your family, and trust there weren’t any; sadly PS babies were lost quite often before the 1950s. I’d be interested to know whether your family is also “strong” in having gastric issues large or small, as the high gastric hormone and acid levels underlying PS tend to continue to be a hazard. But, like me and countless others, you are a survivor – and more! Best wishes.
It was not until today that my new primary physician started talking about a possible link between my pyloromyotomy and the numerous GI issues I have suffered with over the past thirty-five years. While we do a few more tests/studies (gluten intolerance and delayed gastric emptying) he asked me to research “late onset complications of pyloromyotomy”/”Pyloric Stenosis and long term effects”. I found a wealth of information – including this Blog.
What an enlightenment. You might say, “the scales fell from my eyes”!
I received my pyloromyotomy in late-February, early-March 1963 in Michigan, USA. My mother cannot recall (now) how old I was – (3-5 weeks old?) but I have heard the stories throughout my lifetime about what happened when the events were still fresh in my parent’s minds. Born on 06 February to a devout Catholic family I was baptized on 24 February as I was so sick they thought I might die – which makes me think it might have been closer to three weeks old.
As with many other patients’ stories I have read, my pediatrician was slow to act [new mother with her first (male) child is just overreacting]. He finally gave in and told Mom to bring me in with a bottle (she was breast feeding). As soon as he observed my significant weight loss and the projectile vomiting (I’m told it was bad – all over the doctor) he had my mom take me directly to the ER where I was rushed into emergency surgery.
Like yours, my scar is vertical just above and slightly right of center to my umbilicus. Fifty-four years later the scar is about 9cm long. After the surgery though my father told me, in one of his colorful Navy phrases, that I was split “stem to stern” but Mom said it wasn’t that bad. I suppose I am fortunate that my scar looks good and is barely noticeable due to my body hair.
I had no issues at all growing up. I could eat anything and I was described as having a “cast iron stomach”. It was not until I was eighteen or nineteen when I started to gain weight that I started to have these issues with nausea and vomiting. I have lost count of the number hospitalizations to receive IV hydration, pain and nausea medications. I have also forgotten the number of EGD’s (Esophagogastroduodenoscopy) I was subjected to over the years. I have been diagnosed with GERD, Peptic Ulcers, Gastritis, etc., etc. I had one GI specialist tell me I have ulcerative colitis after my first colonoscopy in 2009 and another gastroenterologist tell me I didn’t after a 2014 colonoscopy. Due to a family history of colon cancer, I have been getting colonoscopies every five years since I was forty-six.
Recently, my condition has gotten MUCH worse. Since November 2016 I have had two ED visits, the latest resulting in hospitalization for 2-1/2 days and another “direct admit” for three days when I went to my primary physician with severe nausea, vomiting and dehydration.
Thank you for the information presented here. I have not gone through all of it but, so far, has been VERY helpful to me.
Thank you for posting something of your PS story here, Greg.
It is heartening for me to know that this blog not only has a solid readership, but even more that it meets real needs like yours: knowing that our challenges are not unique nor imagined, but part of a pattern – and that as such we are part of a community learning and networking to make the best possible sense of what we are experiencing, and exploring the best way forward.
You have certainly had a rugged time with your digestion. When I wrote my story, I did not emphasize enough what has become ever more clear: PS is not unrelated to high levels of gastrin (a blood hormone that controls digestive function) and as a result, of gastric acid. Not all medical people admit this is significant but it’s the lifetime conclusion of Dr Ian Rogers, and to me the most persuasive argument I’ve seen.
It follows that although the surgery corrects the pyloric blockage it does not change this high acid output. This in turn explains why the incidence of a list of gastric issues is so common among us! Your problems are all on that list, I’m afraid, although most of us will be grateful we have not had the major problems you are having.
Your fellow PS survivors hope and pray that you and your helpers will get greater clarity and better management of your present situation.
Dear Fred,
Thanks for sending me the blog. Thought you might be interested in this latest offering to Acta Paediatrica.
Best wishes to you and Helen.
Ian
________________________________
So glad you are finding information to help you. Sounds as if you’ve been ‘through it’ as they say.
Fred, I am also a ps survivor, the youngest of 6, female – which is why surgery was delayed until I had what they call “pyloric waves” due to severe dehydration (Mom tried to tell them). Born in early October 1962, surgery in late November 1962, my scar is horizontal and lies just below my right rib cage. Always wore a one piece bathing suit… you know why. I had two first cousins (both male) diagnosed with ps, one had surgery, one did not, also a distant cousin, not sure if surgery was performed. My oldest daughter bore 3 sons, the first one was premature, but the second one was diagnosed with ps and required surgery around 6 weeks of age (now 21 years old), he suffered with some learning and separation issues. Unique to me (that I’ve not seen mentioned in other posts) is that whoever I left the house with carried a list of food NOT TO LET ME EAT: Graham crackers, oatmeal, chocolate, raisins, and a few others that have escaped me in the last 50 years. I would have uncontrollable diarrhea (I remember running home from the playground in tears – talk about humiliating). I truly believe that caused me to have some life-long social issues. But then I got fat… must have been about 9 years old. In adulthood, weight has been a constant struggle… basically starving and self-medicating to ward off weight gain. Most recently… (within the last year) my abdomen is very distended and I’m very uncomfortable. Starting with a fresh round of doctors but will always wonder if my life saving surgery left me with some later in life damage.
p.s.(no pun intended) I have a brother named Fred (and none of my 5 siblings had ps).
Thank you for telling some of the details of your experience with PS, Cindy. It is much appreciated and adds value to all the voices here.
You have benefited from having a good bit of your story passed on to you by your family: how I urge parents to keep the records, photos and anecdotes relating to their baby’s illness and surgery. Having had surgery as a baby seems unreal to many people in our position, and I regret that my hated scar is my only memento.
You have not been helped by your rather unstable digestive system: wow! I also have not come across another PSer who was accompanied in their childhood by a list of dietary restrictions, although I can imagine you would not be alone. My mother always protected me a bit because she knew me as “”a sensitive child” – something similar perhaps?
I imagine the weight issues you mention are part of your inherited constitution? Some have recognized a clear link between their PS and either over- or under-weight problems. Whatever, I do know that PS itself (quite apart from the surgery) leaves us with high gastric acid levels which cause unstable bowels, reflux and/or IBS, and other possible troubles.
And you have a brother Fred! Quite a common name when I was a kid, but I don’t know any who are much younger than I!
Best wishes!
I had PS surgery at 2 months in 1957. My mother told me that I was very thin and dehydrated and kept vomiting. The doc told her to stop breast feeding and to switch to soy milk. Nothing was working so finally the surgery was done. I have a diagonal scar on the right side. I also had ankle scars from the surgery, from putting the lines in since I was so dehydrated. I don’t have any adhesions. I have 2 other scars from a ruptured appendix and have had more trouble with those scars than the PS scar. I was very self-conscious about this and other scars and spent way too much time trying to find the right bathing suits. I kind of lost that self-consciousness when I was a teenager. I am normal weight but have IBS. That may have been due more to my anxiety. I do have PTSD and Generalized anxiety disorder. I have thought possibly the early trauma may have contributed to this. I did not bond with my mother and did not feel attached to her throughout childhood. There were other factors besides the PS, As an adult, we had a respectful relationship. I wonder if the PS problem contributed to this lack of attachment. I also have a very difficult time with medical professionals, procedures, sensory issues.
Finally, I passed on this gene to my first born son. When I observed the projectile vomiting, I told my doctor that I had PS and he agreed to the surgery. He had observed my son vomit his feeding across the room. At 3 weeks, he was thin and dehydrated. He had the surgery at 3 weeks and within a day, he was doing well and gaining weight. His scar became infected so he formed adhesions under the scar. He had a scar revision done at 5 which helped somewhat. He still has some pulling there and says that he can’t eat very much. At 27 yrs. of age, he is very thin (6′, 138 lb). He has always been thin and forgets to eat. He has had similar sensory problems as I have, but does not have PTSD. I don’t think the attachment and trauma issues have to develop with the PS surgery, but if there are other conditions in addition to the PS, I think it may make it more likely. Just my opinion, not based on fact. Thank you for this blog.
Thank you Kelly for your appreciation of my blog, and for writing up here some of your own struggles with your own and your son’s experience with PS.
I recognize so much of myself in what you wrote about your own journey, as you clearly did reading my account. I am so grateful for this kind of sharing and interaction in recent years, as it has done more for my self-understanding, reassurance and healing than what I was able to discover during all my pre-internet years!
Like you, I will never be sure of the reason for some of my trauma symptoms, but I do know that in my case my early surgery, separation, and the effect this had on my parents and me are the only traumatic events and situations in my life, and like you (as I think I wrote) I’ve also had issues with my mother and a longtime fear medical people, procedures and places. Go figure!
I’d be interested to know whether your experience was able to benefit your son’s dealing with similar issues, or whether the mother-son relationaship or other inter-generational issues hampered this.
Best wishes!
Dear Kelly,
My story looks a lot like yours, Kelly. I was only two weeks old and was operated on without anesthesia for PS in the OLVG Hospital in Amsterdam. I too have the big scar on the belly and the two on the ankles. As my parents had a business of their own and another child at home, my father just brought the bottle of mother milk to the reception of the hospital. My father just saw me once in those 6 weeks, behind a window, my mother never came. I too have PTSD and an anxiety disorder. I think that’s due to the early operation without the anesthesia and not having been comforted by parents, especially my mother. I too did not bond with my mother, in fact I struggled in bonding with whoever. It helped a lot for me growing older, searching all I could find about the development of the brain in early childhood and to write my life story. I have 3 children and none of them had PS. Fred, do you know if it can skip a generation, this far I have 1 grandson and he has not had PS.
Fred, thanks for this blog, I have always searched for more info. (Hope my English is sufficient to understand my story 😉
Hi Thea,
Thank you for telling us something of your story, and I assure you that your English is very good, and a bit better than my Dutch!
I was again amazed by how similar many of our older PS stories are, also comparing with some of those I find on the Facebook PS Groups’ pages. Thankfully, the PS babies of the last 30 or so years have received safe and effective anesthesia, have been cared for in hospitals and by parents and surgeons far more aware of the possible psychological effects of infant and parent trauma, and are much more aware of the vital importance of maternal bonding with a newborn baby.
Your post has prompted me to update “My Story” with a few recent observations and a telling experience of two weeks ago. I cannot know with certainty which of several possible factors have triggered the lifelong problems I have had, but know there is a link (or 2 or 3) there – and was heartened to find this medically confirmed!
To answer your question, only about 20% of infant PS is clearly familial. I have 4 children and 11 grandchildren, and PS has not shown up. But yes, my Facebook network includes several stories of PS skipping a generation, sometimes twice over 5 generations! Gastric problems (reflux, IBS and ulcers) are represented on both sides of my Dutch family, and I believe that high gastric acidity and anxiety more than genetics are the common thread that gave me PS.
Hi Thea,
Thank you for sharing your story in replying to Kelly. I too have had PS surgery, which deeply affected my bond with my mother. My surgery was in 1952. Parents were not allowed to see their sick babies back then. My mother visited quite often by sitting in a hallway and observing me through a window. I was 26 days old when the surgery was performed and I was not administered, in all likelihood, anesthesia or pain control. My medical records have been destroyed, but my Post-traumatic Stress symptoms all point to the fact that I had no anesthesia. My relationship with my mother got better once I worked on it intensely in psychological therapy for many years and with our both maturing. I have had difficulty with intimacy due to the broken early attachment, but I was lucky to work through much of this problem in the therapy I mentioned and also in EMDR (Eye Movement Desensitization and Reprocessing) therapy more recently. You say, Thea, that you wrote your life story. Have you gotten it published? I’d like to read it. In any case, so glad you wrote and shared your story. It always helps to have company–to know that others, too have experienced much that is similar to my own experiences in the aftermath of infant surgery without anesthesia. Btw, how did you learn that your PS surgery was performed without anesthesia? I didn’t understand this about my own surgery until I was fifty years old. My mother always said I had anesthesia but in the old days, the paralytic drug was considered ‘anesthesia.’ Would love to hear back from you. Again, thank you! Fyi, I wrote over three hundred blog posts on my website http://restoryyourlife.com, most about healing from preverbal PTSD. Maybe there’s something there that might be of interest to you. Warmly, Wendy
My son had PS surgery at 9 weeks old. We had a mis-diagnosis of reflux at 5 1/2 weeks old, After many upsetting weeks of profuse vomitting I attended my gp in floods of tears and begged them to do something as I knew there was something terribly wrong with my child, He was losing weight and I could see lumps travelling down his tummy. Finally he was diagnosed with ps and had surgery. The surgeon said he had quite a severe ps but he recovered very quickly.
He is 3 1/2 now, He is a very anxious child and extremely irritable and he also has a really bad appetite – we struggle daily with food. He asks for something to eat and I offer several option but he doesn’t like anything. He gets upset that he is hungry but won’t eat anything that is offered to him. He is a very loving child but I really feel there is something that causes his mood swings and I often wonder has it to do with his PS condition or surgery
I wrote a book on PS with Dr Fred and I am happy to send you the electronic version. Basically too much acid in infancy is the cause which is especially troublesome in infancy. However, it may still be bothering him and I would suggest you ask your hopefully improved GP to prescribe for a short time PPI drugs to see if it helps his eating. My email is irogers2000@hotmail.com and I can email you the book. Your GP might like to buy it on the net.
Ian FRCS FRCP PGCMed EDu.
Lorna, I hope that the Comments I have made to Joanna today may also help you in addition to Dr Rogers’ remarks. The relationship between 1) the kind of problems that come with PS (incl. the high acidity Dr Rogers has mentioned), 2) the possible long-term effects of the surgery, and 3) the actual physical and emotional make-up of your son is obviously very complex.
It does make sense to look for a possible connection between his emotional behavior and his early life experience, but keep your mind open as you do this, of course! Light may be shed by 1) cross-checks and comparisions with his genetic kith-and-kin, 2) learning what you can about your son’s experience of PS and its surgical repair and the possible issues around that (incl. complications from the surgery, maternal separation, length and nature of hospital stay – what records and memories do you have?), and 3) getting to know how your son ticks. Life is full of exploration and discoveries! Talking with a good child psychologiest may also help you all.